Evolution of varicose veins treatment
Varicose veins are enlarged, dilated and tortuous veins found in the lower limb. These might not cause pain.
- Veins may appear dark purple or blue.
- Veins may appear twisted and bulging, often appearing like cords on the legs due to chronicity.

When painful signs and symptoms of varicose veins occur, they might include
- A heavy feeling in the legs,
- Burning, throbbing, muscle cramping and swelling in the lower legs,
- Worsened pain after standing for a long time ( gravity worsens pain)
- Itching around one or more of the veins,
- Changes in skin colour (dark pigmentation) around a varicose vein,
- Venous non healing ulcer on the shin or ankle,
- Bleeding from the burst dilated vein or incompetent perforator.
Spider veins are similar to varicose veins, but they’re smaller. Spider veins are found closer to the skin’s surface and are often red or blue and less tortuous.
Spider veins occur on the legs but can also be found on the face. They vary in size and often look like a spider’s web.They are a cause of cosmetic concern.
Aetiology : Causative factors
Weak or damaged valves can lead to varicose veins. Arteries carry blood from the heart to the rest of the body. Veins return blood from the rest of the body to the heart. To return blood to the heart, the veins in the legs must work against gravity.
Muscle contractions in the lower legs ( calf muscles = peripheral heart) act as pumps, and elastic vein walls help blood return to the heart. Tiny valves in the veins open as blood flows toward the heart, then close to stop blood from flowing backward. If these valves are weak or damaged, blood can flow backward and pool in the veins, causing the veins to stretch or twist, compounded by the force of gravity.

Age
Ageing causes wear and tear on the valves in the veins that help control blood flow. Eventually, those weakened valves allow some blood to flow back into the veins, where it collects.

Sex
Women are more likely to develop the condition. Hormonal changes before a menstrual period or during pregnancy or menopause might be a factor because female hormones like oestrogen tend to relax vein walls. Hormone treatments, such as birth control pills, might increase the risk of varicose veins.

Pregnancy
During pregnancy, the blood volume in the body increases. This change supports the growing baby but can also enlarge the veins in the legs. Also the major veins in the abdomen like the inferior vena cava and the iliac veins are compressed by the growing foetus during pregnancy.

Family history
If other family members had varicose veins, there’s a greater chance for the kith and kin to have the same (genetic factor).

Obesity
Being overweight puts added pressure on veins.

Standing or sitting for long periods of time
Movement helps blood flow. Sedentary jobs or jobs involving prolonged standing escalates this disease.
Complications
Complications of varicose veins occur when the disease becomes chronic and the patient has neglected the treatment protocol like wearing of TED stockings and regular calf muscle exercises. Complications include:
- Ulcers : Painful ulcers can form on the skin near varicose veins, particularly near the ankles. A discoloured spot on the skin usually is a harbinger before the skin breaks and before an ulcer forms.This ulcer will not heal with antibiotics or antiseptic creams.
- Blood clots : Occasionally, veins deep within the legs become enlarged and might cause leg pain and swelling. This persistent leg pain or swelling can be a sign of a blood clot or deep vein thrombosis.
- Bleeding : Occasionally, veins close to the skin burst. Although this usually causes only minor bleeding, it may be alarming and cause a patient to rush to the Emergency room..

- Bleeding : Occasionally, veins close to the skin burst. Although this usually causes only minor bleeding, it may be alarming and cause a patient to rush to the Emergency room..
Prevention
Improving blood flow and muscle tone might reduce the risk of developing varicose veins. The same measures that treat the discomfort from varicose veins can help prevent them. They are the following:
- Avoiding high heels,
- Changing your sitting or standing position regularly,
- Eating a high-fiber, low-salt diet,
- Exercising regularly.
- Raising your legs when sitting or lying down (leg elevation)
- Keeping your weight in control

Diagnosis
Spot diagnosis by a trained clinician can detect varicose veins by simple clinical examination.
Bedside clinical tests used to detect the site of reflux, such as palpation for a retrograde transmitted impulse from the saphenofemoral junction through the long saphenous vein (tap test) or for transmission of a thrill or impulse with coughing at the saphenofemoral junction (cough test), are of limited value because of their poor sensitivity or specificity.
Venous colour doppler ultrasonography will detect saphenofemoral and saphenopopliteal incompetence if present and highlight the incompetent perforators.
Spider veins are similar to varicose veins, but they’re smaller. Spider veins are found closer to the skin’s surface and are often red or blue and less tortuous.
Treatment
1. Conservative medical management for stage 1 Varicose veins where this is mild cosmetic concern and the patient is asymptomatic. This includes compression stockings below knee or sometimes above knee length TED stockings as per individual case. Analgesics can be prescribed as per the severity of pain as and when needed,
2. Traditional surgical technique of varicose vein stripping and ligation in which a metallic wire ( Mayo’s stripper) is inserted along the entire length of the greater saphenous vein and the entire vein is stripped or pulled out in one piece with a concertina effect. The surrounding tributaries are ligated flush with the saphenous vein. This is a time tested method but slowly becoming obsolete.
3. Sclerotherapy is an added armamentarium for the treatment of varicose veins. Here one injects a foamy white solution directly into the veins which causes the vein to scar and close.Today the two most common agents used in modern sclerotherapy are sodium tetradecyl sulphate (Sotradecol) and polidocanol (Asklerol).
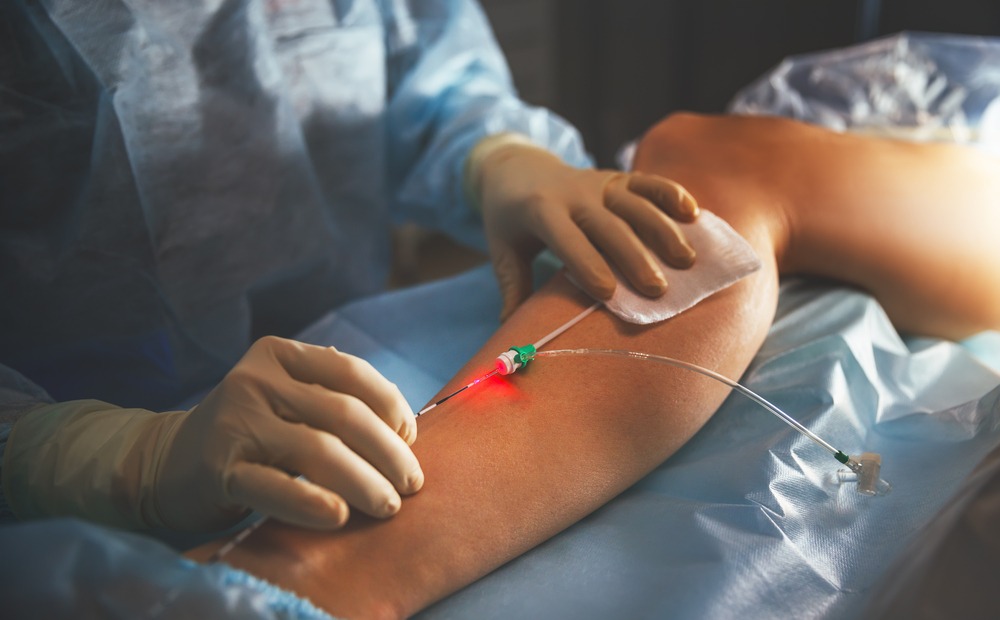
4. Endovenous Laser ablation has replaced RFA or radio frequency ablation therapy due to its accuracy and lesser side effects. The heat kills the walls of the veins and the body then naturally absorbs the dead tissue and the abnormal veins are destroyed.Collateral circulation ensures that the closure of the lasered vein does not hamper the venous return from the legs to the heart.
5. Vena glue is the latest addition in the modalities available for the treatment of the varicose veins patient. A surgical glue like venaseal is injected directly into the vein stepwise while withdrawing the catheter slowly intermittently. This is a painless procedure. It is expensive but coming in vogue rapidly.

3. Sclerotherapy is an added armamentarium for the treatment of varicose veins. Here one injects a foamy white solution directly into the veins which causes the vein to scar and close.Today the two most common agents used in modern sclerotherapy are sodium tetradecyl sulphate (Sotradecol) and polidocanol (Asklerol).
4. Endovenous Laser ablation has replaced RFA or radio frequency ablation therapy due to its accuracy and lesser side effects. The heat kills the walls of the veins and the body then naturally absorbs the dead tissue and the abnormal veins are destroyed.Collateral circulation ensures that the closure of the lasered vein does not hamper the venous return from the legs to the heart.
5. Vena glue is the latest addition in the modalities available for the treatment of the varicose veins patient. A surgical glue like venaseal is injected directly into the vein stepwise while withdrawing the catheter slowly intermittently. This is a painless procedure. It is expensive but coming in vogue rapidly.
For more details our helpline can be reached via Whatsapp + 91 9429616096 or drop an email to ok@drsureshbhagia.com and your queries will be resolved soon.